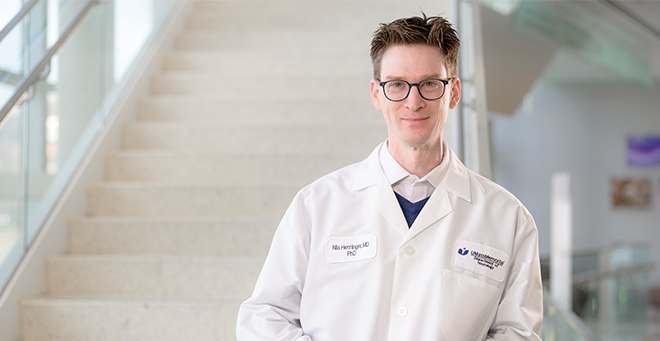
A UMass Chan research team led by Nils Henninger, MD, PhD’18, associate professor of neurology and psychiatry, recently published a study that sought to untangle the interplay between traumatic brain injury and genetic predisposition for risk of developing frontotemporal dementia and amyotrophic lateral sclerosis.
FTD and ALS are fatal neurodegenerative diseases that represent ends of the spectrum of a single disease. The most common genetic cause of FTD and ALS is a mutation in a gene called C9ORF72. Disease onset and duration are highly variable and epidemiological studies suggest that environmental factors, including traumatic brain injury, may affect its onset and course, but the role isn’t well understood.
Findings from the new study, which was published in Brain, indicate that repeated traumatic brain injury can be an environmental risk factor that is sufficient to trigger ALS- and FTD-associated changes and behavioral deficits in mice carrying the C9ORF72 gene mutation.
“Understanding this link and establishing a model system like we have is critically important to have as a foundation for the next step, which is to understand specifically what is driving diseases; and then in parallel, to see if we can stop that disease process by therapeutic intervention,” said Dr. Henninger.
The study looked at motor abilities, behavior and tissue markers in mice that were modeled with the mutation in the C9ORF72 gene. In the absence of traumatic brain injury, these mice did not show symptoms of disease. Mice that did not have the gene mutation served as a comparison.
In each group of mice—those with genetic predisposition and those without—some were subject to the repeated traumatic brain injury procedure, while the others received a sham procedure. The mice were then observed for 12 months.
“Understanding this link and establishing a model system like we have is critically important to have as a foundation for the next step, which is to understand specifically what is driving diseases; and then in parallel, to see if we can stop that disease process by therapeutic intervention.“
The scientists found that repeated mild traumatic brain injury increased the time to recovery from anesthesia, reduced grip force—a motor behavior—and altered certain sociability behaviors in mice with the genetic predisposition for FTD/ALS. They also found that by one year after repeated brain injury these genetically modeled mice exhibited widespread microglial activation, suggesting heightened immune response and persistent neuroinflammation.
Importantly, the animals had a reduced density of neurons, axons and synapses in the cerebral cortex, which was associated with the pathological accumulation of a protein that is a major hallmark of the genetic mutation in humans. In contrast, these pathologies were not found in mice that did not have the genetic mutation and were not subject to repeated mild brain injury.
“A big goal of our study was to establish whether the combination of traumatic brain injury and the most common genetic background for ALS/FTD could trigger neurodegeneration including the loss of neurons, axons and synapses as well as pathological accumulation of the associated protein; and that, to my knowledge, has not been shown before,” said Henninger.
The implications of this research may extend beyond ALS and FTD, according to Henninger. Many of the pathologies seen in this model are also seen in other neurodegenerative diseases characterized by cognitive decline and dementia such as Alzheimer’s disease and chronic traumatic encephalopathy, which is a brain condition thought to be linked to repeated head injuries, including sports-related collisions.