The ability to detect if patients are taking their medications for opioid use disorder is the driving force behind a wearable device being developed at UMass Chan Medical School in collaboration with the Wearable Biosensing Lab at the University of Rhode Island. The goal of the device is to help improve medication adherence and prevent overdose deaths.
Called the MINDER-band, the upper-arm device will use an artificial intelligence-assisted sensor system that will continuously monitor physiologic changes and data to accurately identify buprenorphine use and withdrawal.
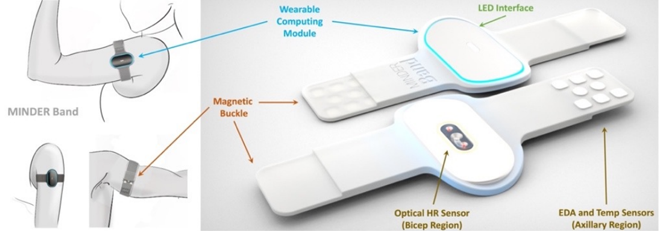
The MINDER system will also include a mobile app and an online clinician-facing portal.
“We identified a clinical problem with buprenorphine, a medication for opioid use disorder that works really well if people take it. For several reasons, people stop taking it, develop opioid withdrawal and go back into the same routines they were in before,” said Stephanie Carreiro, MD, PhD'22, associate professor of emergency medicine and principal investigator on the development of the MINDER system.
“So we designed a device that can help identify when people are in withdrawal or when they haven't taken their medication,” said Dr. Carreiro.
In the future, the MINDER device will use notifications to alert clinicians that a patient might need extra support or positive reinforcement, such as supportive interventions, to ensure patients are adherent to their buprenorphine as prescribed.
Carreiro received a $2.6 million award over four years from the National Institute of Biomedical Imaging and Bioengineering to support the development of the device.
During the first year of the grant, the team will focus on the development of the arm band and gather feedback from people who use medications for opioid use disorders to make sure their needs are being met with the device. This summer, they will conduct focus groups with clinicians and interviews with patients.
Over the next three years, investigators will focus on putting the device on people in a lab setting and having them take their medication in the lab for evaluation.
“The lab work will help us tweak our algorithms to make sure that we can use that data to understand when people take the medication and what they're feeling in terms of withdrawal. Then we're going to deploy it in the outpatient setting, put the MINDER-bands on people who are at home taking their medications and have them video themselves taking the medications,” Carreiro said. “That data will help develop the app that will go with the arm band and then it will be ready for interventions and clinical trials.”
Carreiro and David Smelson, PsyD, professor of psychiatry and director of the Center of Excellence in Addiction, are overseeing the clinical testing, patient recruitment and data collection for the MINDER system. At the University of Rhode Island, Kunal Mankodiya, PhD, associate professor of electrical, computer and biomedical engineering, Dhaval Solanki, PhD, assistant teaching professor of electrical, computer and biomedical engineering, and Krishna Venkatasubramanian, PhD, assistant professor of computer science and statistics, are developing the MINDER device and application.

