New research by Kaleido Biosciences, Inc., and UMass Medical School investigators John P. Haran, MD, PhD, and Beth McCormick, PhD, shows that the company’s microbiome metabolic therapy candidate produced positive results in patients with mild-to-moderate COVID-19. The analysis showed a reduction in overall hospitalizations, emergency room visits and urgent care visits related to COVID-19.
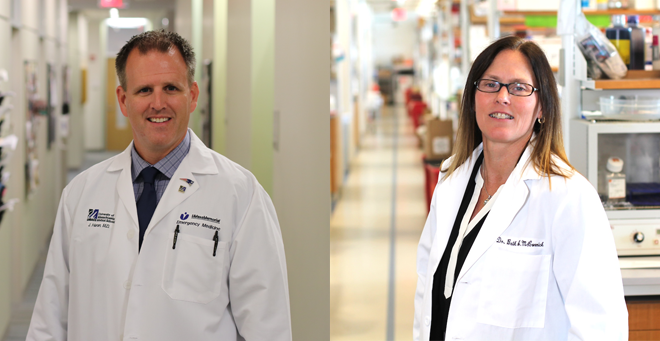
Dr. Haran, associate professor of emergency medicine and microbiology & physiological systems, is clinical director of the UMass Center for Microbiome Research. Dr. McCormick, the Worcester Foundation for Biomedical Research Chair and professor and vice chair of microbiology & physiological systems, is founding director of the Center for Microbiome Research.
The study also demonstrated a significant reduction in recovery time for patients age 45 and older or with one or more comorbidities who received the product, named KB109, plus self-supportive care as compared to patients receiving self-supportive care alone. KB109 also demonstrated an overall favorable safety and tolerability profile with no unexpected treatment-related adverse events.
Kaleido’s microbiome metabolic therapies are similar to a prebiotic. They are designed to feed and promote the healthy bacteria in the gut. They drive the function and distribution of the microbiome’s existing microbes in order to decrease or increase the production of metabolites, or to advantage or disadvantage certain bacteria in the microbiome community.
“The data released from Kaleido Biosciences are highly impressive and I believe represent an exceptional advance,” said Haran. “Oral therapies that reduce the duration of symptoms in patients with COVID-19 are in great need and would offer much needed therapeutics to patients suffering from the long-lasting effects after infection. If these data are replicated in a pivotal drug study, they would represent an opportunity for an oral therapeutic targeting the microbiome—the trillions of microbes living inside our bodies—to reduce health care utilization and accelerate patient recovery from COVID-19.”
COVID-19 infection has been associated with activation of an inappropriate inflammatory cascade that in some patients can cause an abnormally aggressive immune response leading to pneumonia and respiratory failure. Metabolites such as short chain fatty acids (SCFAs) produced by the microbiome through utilization of glycans are modulators of the immune response and therefore could play a role in limiting this inflammatory cascade.
In preclinical models, increased SFCAs and/or SFCA-producing taxa have been shown to influence immune pathways, mitigate immune pathology and improve survival and morbidity associated with severe respiratory viral infections.
Human data also support the role of SCFAs in reducing the impact of viral infections. In patients undergoing hematopoietic stem cell transplants who have contracted respiratory viral infections, including coronavirus, the presence of SCFA-producing taxa has been associated with a significantly reduced risk of progression to lower respiratory tract infections, which can have substantial morbidity in this patient population.
The study was a multi-center, open label, controlled non-IND (non-investigational new drug) clinical study of 350 patients in which 181 received KB109 plus self-supportive care and 169 received self-supportive care alone. KB109 is a novel, orally administered product candidate based on the Kaleido’s microbiome metabolic therapy (MMT) platform.
“Despite historic progress in advancing COVID-19 vaccinations, new strains of the virus continue to emerge, necessitating safe, orally available therapies for patients around the world,” said Dan Menichella, president and chief executive officer of Kaleido Biosciences. “Based on these results, we are excited to advance KB109—which can be administered at home—into an IND to assess whether it may help improve patient outcomes, particularly among more vulnerable populations.”
“Because KB109 is designed to affect the host’s immune response, rather than the virus itself, we believe it may produce a similar response to virus variants or other types of viral respiratory infections,” Menichella said, “With the goal of moving into a pivotal registration program in mild-to-moderate COVID-19 patients who are at risk for prolonged symptoms, we look forward to filing an IND application with the FDA and a Clinical Trials Application with other regulatory agencies.”
As a non-interventional extension to the completed study, Kaleido is continuing to study the impact of KB109 on the incidence of “long-COVID,” an emerging concern in which symptoms of the virus persist in patients for weeks and months.
Related story on UMassMed News:
Beth McCormick, John Haran work with Kaleido Biosciences to explore link between microbiome and COVID-19