Alpha-one Antitrypsin Deficiency Lung Disease
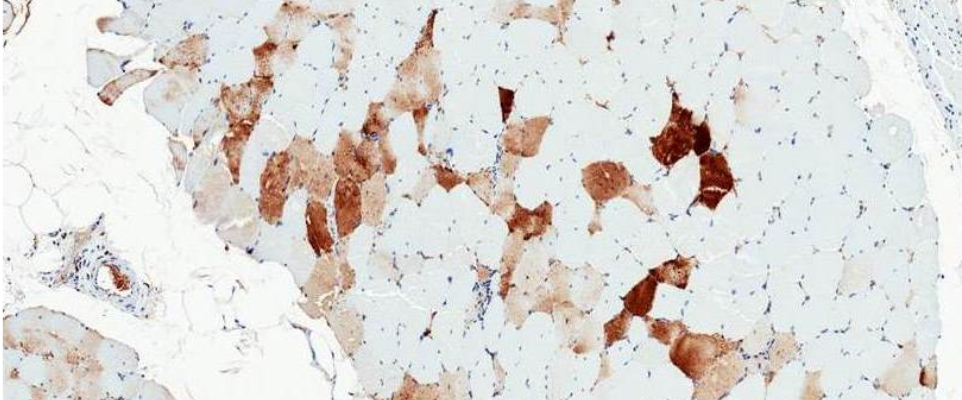
This image shows muscle tissue where individual muscle fibers can be identified. This muscle biopsy comes from a patient who received intramuscular injections of a gene therapy vector expressing AAT as part of our clinical trial. The brown color indicates presence of AAT protein. As AAT is not normally expressed in muscle, the presence of the protein is vector-related.
What is alpha-one antitrypsin (AAT) deficiency lung disease?
AAT deficiency occurs worldwide, but the prevalence is variable depending on regions. It is a rare disease in Europe and in the US. It affects between 1:1500 and 1:3500 in people of European descent. It is the 2nd most common genetic disorder in Ireland, where 1:25 people carry the mutant gene. It is rare in Asians.
AAT deficiency lung disease is caused by low levels or complete absence of serum AAT (also called M-AAT).This is due to mutations in the SERPINA1 gene which contains the information to produce the AAT protein. Several mutations have been identified, and the most common ones are called Z and S, where mutant proteins Z-AAT and S-AAT are expressed. There is also a null phenotype, where absolutely no protein is expressed.
AAT is produced by the liver, released into the bloodstream where it travels to the lungs. There AAT protects the lung alveoli from a powerful enzyme called neutrophil elastase. The physiological role of neutrophil elastase is to protect the same alveoli from infections and harmful irritants; the enzyme then gets inactivated by AAT. However in the absence or lower abundance of AAT, elastase will attack the lung tissue itself, causing irreversible damage.
Clinically this leads to shortness of breath, asthma-like symptoms, decrease in respiratory function and ultimately emphysema. Patients whose lung function is highly affected will be in need of a lung transplant. The current standard of care is weekly or biweekly intravenous infusion of recombinant protein. However this lifelong treatment can be a burden for the patients, and therefore novel therapeutics that would allow for less frequent interventions are being actively investigated. These therapeutic strategies include gene therapy and genome editing.
Our therapeutic strategy: augment serum AAT levels with gene therapy
We aim to augment serum AAT levels following intramuscular injection of an AAV1 vector expressing AAT. The main advantage of gene therapy over recombinant protein augmentation therapy is that it would be a one-time treatment, as opposed to weekly or biweekly infusions.
This strategy has already been tested in clinic trials. We showed that the transduced muscle fibers do express AAT, which is normally not present in muscle tissue (see image on top of this page). Unfortunately, in our first trial the serum AAT levels that were achieved in the patients were too low to be therapeutic. However, we have since then generated a second generation vector that is much more potent in preclinical studies, and we are hoping to move this forward in the near future.
In this research area we are partnering with Dr. Terence Flotte. For more information, you can visit his website here.
NEW! The first mouse model of alpha-one antitrypsin deficiency
We are excited to announce that we recently generated the very first mouse model of alpha-one antirypsin deficiency lung disease and that we will very soon be ready to share it with the research community.
There never was a mouse model before because while there is only one SERPINA1 gene in humans, there are six Serpina1 genes in mice. However CRISPR technology now made it possible to generate this model and disrupt all genes. It has a normal lifespan and its phenotype recapitulates the human disease.
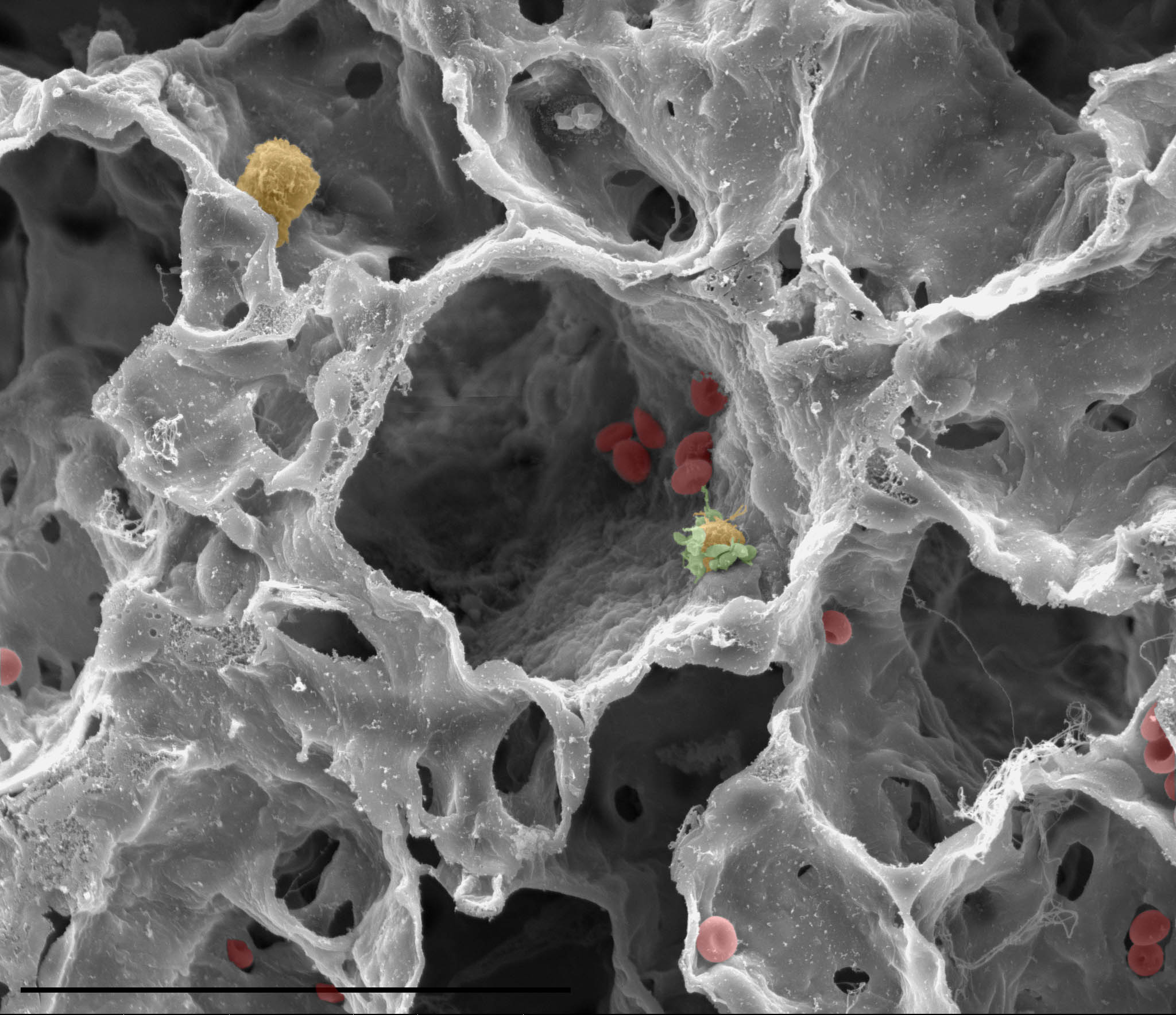
This model will be the ideal setting for studying AAT deficiency and validating new therapeutics for AAT deficiency, because it recapitulates the human disease very well. This model will also be useful to researchers studying emphysema and chronic obstructive lung disease (COPD). COPD affects about 10% of the world population and is the third leading cause of death. Cigarette smoking and environmental factors are major risk factors. But did you know that AAT deficiency is the most common genetic factor for COPD?
If you are interested in using this model, please contact us!
Let's have the next breakthrough together!