Projects
Mechanisms of Conductive Presbycusis In Humans (Remenschneider NIH/NIDCD K08)
Age-related high frequency hearing loss (presbycusis) is a near universally experienced condition, affecting tens of millions of individuals in the United States alone and costing worldwide more than $750 billion per year. Presbycusis results in difficulty understanding speech, problems hearing environmental sounds and, if unaddressed, can lead to social isolation. Given current demographic trends, the societal burden of presbycusis is expected to accelerate. Despite the prevalence of presbycusis, much remains unknown about its etiologic mechanisms. Presbycusis has long been assumed to be secondary to sensorineural dysfunction, but emerging evidence suggests conductive pathology contributes to presbycusis.
 Conductive Presbycusis
Conductive Presbycusis
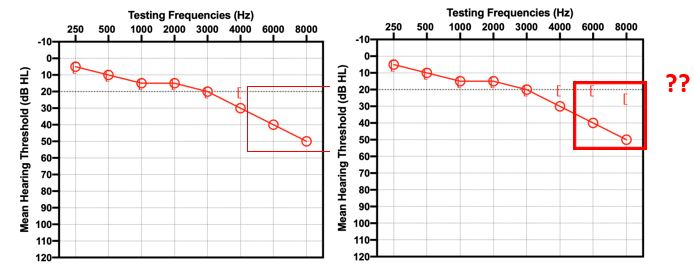
Figure 1. Current methods of clinical audiometry are incapable of reliably distinguishing conductive from sensorineural pathology at high frequencies. Our primary research objective is to establish new methods for measuring bone conduction thresholds at high frequencies, thereby better localizing the origins of age-related high frequency hearing loss. In this example audiogram, the lack of bone conduction thresholds at 6 and 8kHz preclude the precise localization of auditory pathology.
The principal method for clinical evaluation of hearing is behavioral pure tone (500-8kHz) audiometry. Extended high frequency air conduction testing (>8kHz) is now commonly performed given new knowledge on the role of high frequency sound for speech understanding and sound localization. Unfortunately, clinical bone conduction testing stops at 4kHz. Above 4kHz, limitations in standard stimulus transducers that are largely unchanged from the 1950s, and a lack of normative bone conduction standards limit study of high frequency conductive loss. Differentiation between sensorineural and conductive presbycusis is not routinely performed, but is of interest because: 1) prior work demonstrates discrete changes within the middle ear can lead to isolated high frequency conductive loss (ie: with normal low-frequency thresholds) and 2) our ability to surgically repair the middle ear. Further investigation into the prevalence and functional significance of age-related middle ear change is necessary to ensure emerging therapies for presbycusis are appropriately directed.
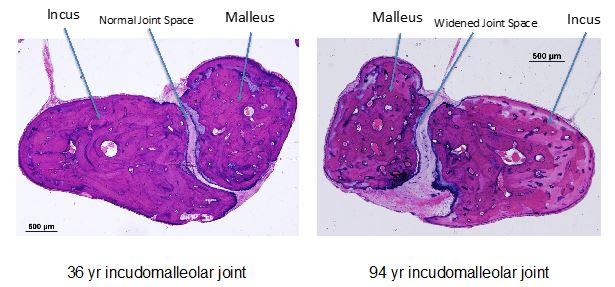 Figure 2: Age-related ossicular joint differences, such as a widened incudomalleolar joint, may result in compliance changes in middle ear sound transmission, and lead to high frequency hearing loss. Through the study of human otopathology, our group has recently identified widened IM joints in cases of indeterminant presbycusis. (Roychowdhury P Otolaryngol Head Neck Surg 2021)
Figure 2: Age-related ossicular joint differences, such as a widened incudomalleolar joint, may result in compliance changes in middle ear sound transmission, and lead to high frequency hearing loss. Through the study of human otopathology, our group has recently identified widened IM joints in cases of indeterminant presbycusis. (Roychowdhury P Otolaryngol Head Neck Surg 2021)
Newly developed bone conduction transducers without high frequency limitations permit comprehensive bone conduction testing at frequencies up to 16kHz. Novel transducers will help to finally establish whether a clinically relevant conductive or mixed presbycusis exists, shedding light on the functional effects of the aging middle ear. Development of reliable testing for high frequency conductive hearing loss carries implications beyond presbycusis, including post-middle-ear-surgery hearing assessment. Our goal is to identify mechanisms of conductive presbycusis and to establish methods to reliably diagnose high frequency conductive hearing loss. We hypothesize that a subset of patients with presbycusis have increased ossicular compliance resulting in conductive or mixed high frequency hearing loss.
Innovative Solution to Tympanic Membrane Repair (Remenschneider DoD SBIR Phase II)
The tympanic membrane (TM), also known as the eardrum, is a complex structure that captures and transmits sound from the environment to the ossicles of the middle ear. TM perforations most commonly occur as a result of chronic ear infections that annually affect more than 30 million children and adults worldwide. The TM may also be injured following direct trauma or blast injuries, as seen in military and civilian populations following terror attacks, such as the Boston Marathon bombings. Perforations produce pain, ear drainage and debilitating hearing loss. The surgical repair of TM perforations is a commonly performed procedure but carries with it variable outcomes, and many patients experience poor wound healing and hearing results. Revision surgery due to graft failure is necessary in up to 30% of cases of TM perforation repair. Surgical failure is thought to be due in part to intrinsic defects of autologous grafting materials, such as muscle fascia and cartilage. Given the paucity of viable alternatives, autologous grafting materials have been used for several decades without significant improvements in patient outcomes. Non-autologous and synthetic materials, including chitosan, alginate, hyaluronic acid and silk fibrin have been investigated as potential alternatives for autologous tissue; however, they have not achieved clinical adoption due, in part, to limitations in materials and design.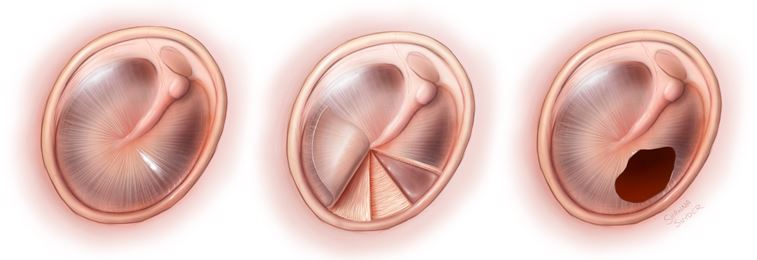 Fig 1. The tympanic membrane (eardrum) is a thin tissue with a highly organized collagen fiber arrangement that is critical to its ability to conduct sound. Unfortunately, it is prone to perforation from blast injury, ear infections or trauma. Eardrum perforations lead to hearing loss, infections, pain and dizziness. (© Shawna R Snyder Illustration 2020)
Fig 1. The tympanic membrane (eardrum) is a thin tissue with a highly organized collagen fiber arrangement that is critical to its ability to conduct sound. Unfortunately, it is prone to perforation from blast injury, ear infections or trauma. Eardrum perforations lead to hearing loss, infections, pain and dizziness. (© Shawna R Snyder Illustration 2020) Fig 2. Traditional methods of repairing eardrum perforations use tissue harvested from the patient. This graft tissue does not match the highly organized structure of the native eardrum and may result in poor hearing outcomes after surgery. (© Shawna R Snyder Illustration 2020)
Fig 2. Traditional methods of repairing eardrum perforations use tissue harvested from the patient. This graft tissue does not match the highly organized structure of the native eardrum and may result in poor hearing outcomes after surgery. (© Shawna R Snyder Illustration 2020)
Recent advances in 3-dimensional (3D) printing allow the creation of structures with impressive complexity on a micron scale. Our group has successfully fabricated novel biomimetic 3D printed TMs that parallel the organized fiber patterns of the human TM. We have determined that by altering the scaffold materials and architecture, specific acoustic and mechanical properties of the TM can be readily modified. Indeed, the printed membranes can be “tuned” to exhibit sound induced surface motion patterns and point velocities similar to the human TM. Further, unlike currently used autologous materials, such grafts maintain shape following mechanical stress. In vitro studies demonstrate printed polymers are biocompatible and promote cellular remodeling in an organized, directed fashion.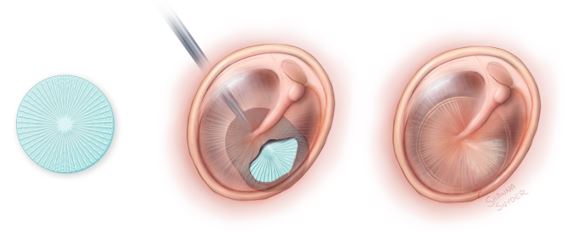 Fig 3. In conjunction with Drs. Jennifer Lewis and Nicole Black at Harvard’s John A Paulson School of Engineering and Applied Sciences, we have developed novel eardrum grafts using 3D printing. These grafts have a biomimetic structure to re-establish the fiber arrangement of the reconstructed tympanic membrane. With control over the specific architecture, we can customize grafts in an effort to optimize healing and hearing outcomes in tympanoplasty. (© Shawna R Snyder Illustration 2020)
Fig 3. In conjunction with Drs. Jennifer Lewis and Nicole Black at Harvard’s John A Paulson School of Engineering and Applied Sciences, we have developed novel eardrum grafts using 3D printing. These grafts have a biomimetic structure to re-establish the fiber arrangement of the reconstructed tympanic membrane. With control over the specific architecture, we can customize grafts in an effort to optimize healing and hearing outcomes in tympanoplasty. (© Shawna R Snyder Illustration 2020)
Our current work focuses on evaluating the functional efficacy of biomimetic 3D printed TM grafts in an animal model. We hypothesize that biomimetic 3D printed TM grafts can safely and effectively repair chronic TM perforations. Moreover, such a TM graft could be placed in the clinic setting, obviating the need for extensive surgical procedures and autologous tissue harvest. Our ultimate goal is to definitively demonstrate the viability, safety and superiority of 3D printed TMs to permit ultimate use in patients.
