Are COVID-19 vaccines and boosters effective if I have lupus?
Created with Biorender.com
As COVID-19 restrictions lift around the world, cases continue to be high. According to the CDC, there are about ~120,000 new COVID-19 cases in the U.S. reported each day, and these reports are severely undercounted1. With the rise of new variants and colder weather on the horizon, you might be wondering what you can do to stay healthy, especially if you are living with an autoimmune condition like lupus.
Systemic lupus erythematosus (SLE) is the most common type of lupus. Lupus occurs when the immune system attacks its own tissues, causing inflammation and tissue damage. Periods of lupus symptoms (aka flares) can be triggered by infection, injury, stress, and occasionally vaccines. SLE is often treated with immunosuppressive drugs that reduce the activity of the body’s immune system. Because of these drugs and intrinsic immune dysfunction, people living with SLE have been reported to have a higher risk of COVID-19 infection and worse outcomes2. As a result, individuals with SLE are among the most vulnerable when it comes to COVID-19.
How do the COVID-19 vaccines work?
The American College of Rheumatology (ACR) recommends the multi-dose mRNA vaccines (Pfizer or Moderna) for individuals with rheumatic disease, which includes people living with lupus3. The initial vaccine series consists of at least two doses of the Pfizer or Moderna vaccine. The ACR also recommends a third dose in the initial series for people who are moderately to severely immunocompromised3. After receiving the initial series, the CDC recommends a booster shot4. Older adults and people who are moderately to severely immunocompromised may receive a second booster, for a total of four or five doses. In addition, both Pfizer and Moderna are working on new boosters that also target new subvariants (Omicron BA.4 and BA.5). These boosters may become available later this fall.
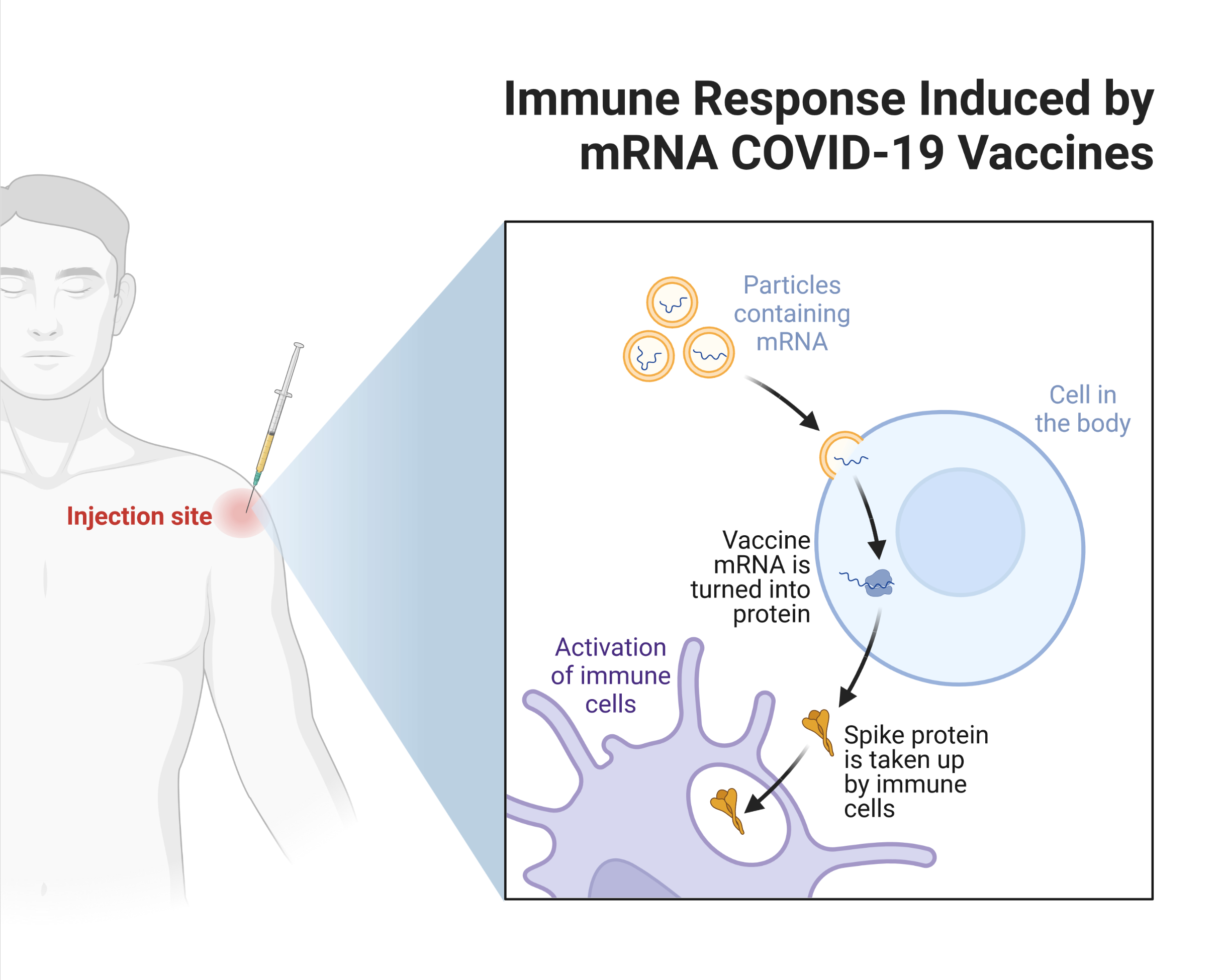
Pfizer and Moderna both use messenger RNA from the COVID-19 virus to give our cells instructions to make a piece of the virus - in this case, the spike protein. After getting vaccinated, our bodies recognize that the protein shouldn’t be there. In response, our immune system starts making antibodies, which are proteins that bind to the virus to prevent an infection. Our bodies also build memory cells that remember how to fight COVID-19 if we get infected. High antibody levels can neutralize the virus and protect against infection. Unfortunately, after a few months, antibody production decreases. Boosters can bump up antibody production so that we stay protected!
Created with Biorender.com
Is the vaccine effective and safe for people with lupus?
Research has shown that individuals with lupus have weaker immune responses and lower antibody levels after two doses of the mRNA vaccine, compared to people without lupus. However, a recent study has shown that people with SLE who had low or no protection after two doses had a significantly improved immune response after a third dose2. The study followed 163 men and women with SLE who had received two doses of the mRNA vaccine. Out of the 163 participants, 125 individuals received a third dose or booster of the same vaccine. Only 22% of the participants with SLE who received a third dose developed a subsequent COVID-19 infection, compared to 42% of those who had not received a booster. These results suggest that the vaccine and booster are beneficial for individuals with lupus2.
Other studies have reported manageable side effects and a low incidence of vaccine-related flares in individuals with lupus. In a survey study of 696 individuals with SLE, only 3% of individuals experienced a medically confirmed SLE flare after vaccination5. Individuals who had a flare in the past year had a higher chance of a flare after getting vaccinated. Overall, the side effects of the vaccine in individuals with rheumatic disease were similar to data from the general population and vaccine trials5.
Will my lupus medications affect how the vaccine works?
Individuals on immunosuppressive medications (i.e., glucocorticoids, methotrexate, mycophenolate/mycophenolic acid, and rituximab) have been found to have a particularly delayed or reduced immune response to the vaccine5. In a recent study, researchers followed 87 people with rheumatic disease who developed COVID-19 infections after being fully vaccinated with two doses of the mRNA vaccine6. 22 individuals developed severe infections that required hospitalization6. Over half of this group that was fully vaccinated and hospitalized had been on an immunosuppressant: 45% were on B-cell depleting therapy (BCDT) at the time of vaccination, and 13% were on mycophenolate6. For comparison, in the overall group of fully vaccinated individuals, only 18% were on BCDT and 11% on mycophenolate. These results indicate that there may be a “blunted” vaccine response associated with immunosuppressant use.
Despite the “blunted” response, a third or additional dose of the vaccine has been found to be effective in increasing antibody levels even in individuals on immunosuppressive therapies2. When a third dose was administered, an immediate increase in antibody levels occurred even in individuals on immunosuppressants who did not respond to the first two doses2. As a result, the COVID-19 vaccine and booster are still important to prevent severe disease, even in those on immunosuppressants.
Besides the vaccine, what are some tips to avoid COVID-19 infection and stay healthy?
As many people living with lupus or other autoimmune diseases already know, mask wearing, frequent handwashing, social distancing, and limiting nonessential travel can reduce the risk of contracting viral illnesses like Sars-CoV-2 (the virus that causes COVID-19). Double masking – wearing a cloth mask over a surgical mask – can also help prevent the spread of the Omicron viral strain. In addition, telemedicine can be a convenient tool to stay safe while continuing to take care of your health. Finally, be sure to prioritize your mental health! It’s natural to feel stress and anxiety during the pandemic, and it is important to stay in touch with your support system and seek additional resources if you’re struggling.
COVID-19 and Mental Health Support Resources:
- Lupus Foundation of America/LupusConnect: https://www.lupus.org/resources/lupusconnect
- National Alliance on Mental Illness: https://www.nami.org/findsupport
- UMass Memorial Center for Mindfulness: https://www.ummhealth.org/center-mindfulness
Sources:
- https://covid.cdc.gov/covid-data-tracker/
- https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(22)00190-4/fulltext
- https://rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf
- https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8586600/
- https://rmdopen.bmj.com/content/8/1/e002187