Center Projects
The Center researchers and trainees are pursuing three collaborative research projects using a combination of clinical, genomic, molecular, CRISPR gene editing and pathway inhibitor studies and our unique patient and animal disease models of FSHD.
Project 1: Genetic Modifiers of FSHD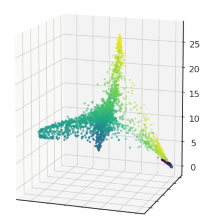
Genetic modifiers of FSHD disease severity will be identified in genome studies of families in a large Utah kindred. A migrating pioneer carried an FSHD mutation into Utah in the 1840s. He had over 18,000 descendants, many of whom inherited the disease-associated D4Z4 repeat contraction and FSHD1 in an autosomal dominant fashion, with variable clinical expression in families. Project goals are to i) document the clinical severity in 300 FSHD and unaffected family members in this Utah FSHD kindred; ii) conduct a genome wide association study (GWAS) of members with disparate clinical severity to identify candidate gene modifiers; and iii) validate genetic modifiers in animal models and replicate family cohorts.
Project 2: FSHD Disease Biomarkers
Genes and pathways that modulate the function of DUX4, the FSHD disease gene, and contribute to DUX4 induced cell death will be identified as actionable targets for FSHD therapeutic intervention. Genome-wide loss-of-function and gain-of-function CRISPR screens of DUX4 inducible muscle cells will identify genes required for DUX4 toxicity. Genes identified in these screens, including the hypoxia pathway genes, and drugs known to target these pathways will be validated in FSHD animal disease models for their efficacy in blocking DUX4 toxicity and disease progression. A second goal is to identify kinases that regulate posttranslational modifications and toxicity of the DUX4 protein, as candidate FSHD therapeutics.
Project 3: Animal Models of FSHD for Therapy Development
Lipid-conjugated siRNAs targeting DUX4 will be developed to identify therapeutics that effectively disrupt the expression and function of DUX4 in patient FSHD muscle cells. Systemic delivery to FSHD patient muscle xenografts in immune-compromised mice will then be evaluated, as a basis for translation to clinical trial evaluation. Additionally, the function of hyaluronic acid signaling in DUX4 toxicity will be investigated using pathway-specific drugs in FSHD patient muscle cell and xenograft models to identify drugs with potencies suitable for in vivo therapeutics in FSHD patients, as a basis for translation to clinical trial evaluation.