Establishing the Contribution of Cytoskeletal Defects in ALS
Why is it important to identify novel ALS genes? One benefit is that it opens up new avenues of research. For instance:
- The identification of some genes leads to new diagnostic tests or eventually gene therapy for a small set of ALS cases.
- The discovery of new ALS genes leads to the essential and much needed development of model organisms that develop ALS when the mutant gene is introduced, providing opportunities to understand the disease that would not be possible otherwise.
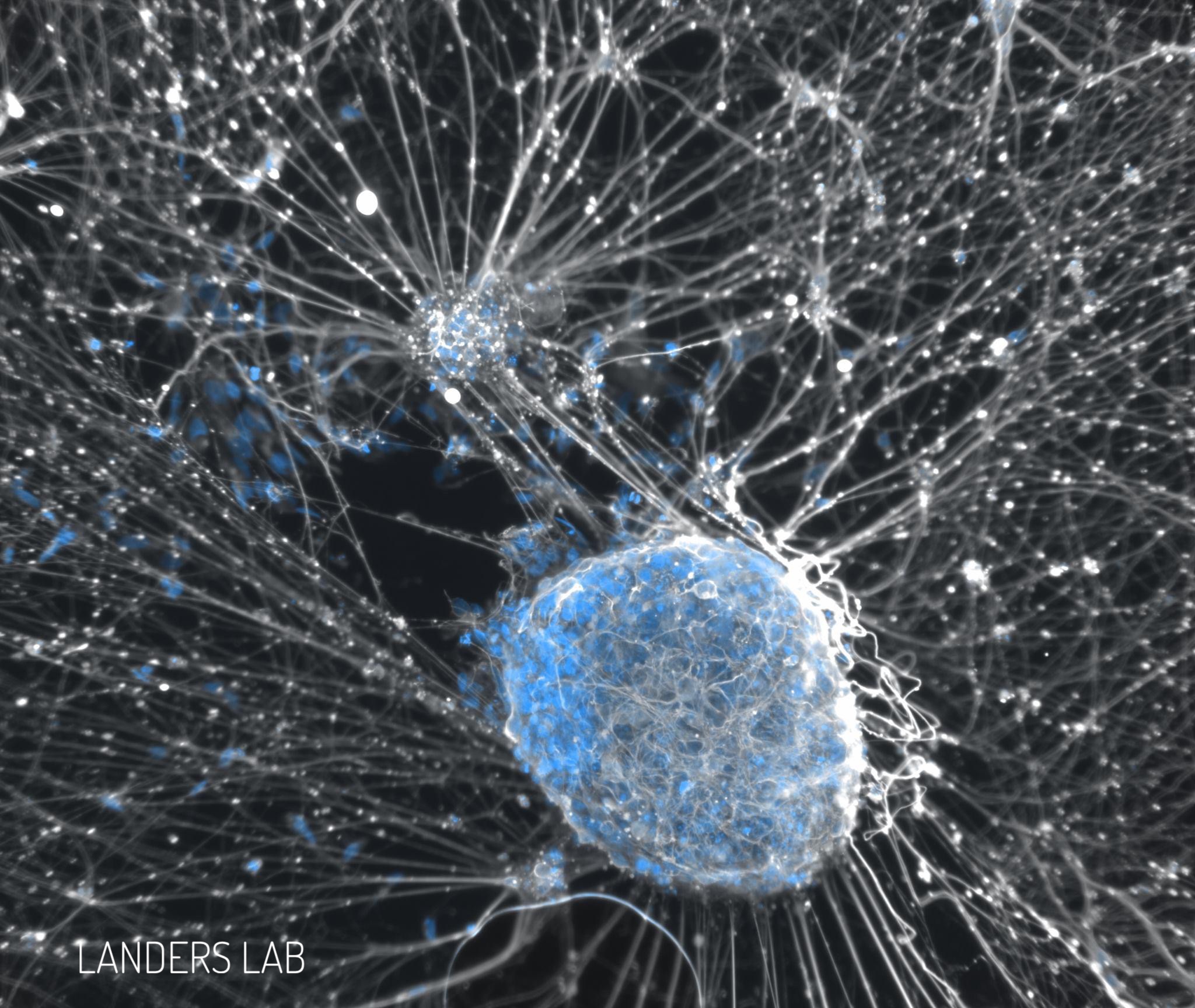
Determining the pathways contributing to ALS pathogenesis is essential for identifying novel targets for therapeutic intervention. Through our genetics efforts described above, we have identified several genes associated with ALS that are tightly linked to cytoskeletal stability and dynamics (PFN1, TUBA4A, NEK1, and KIF5A). The cytoskeleton is a vital component to all cells but especially neurons. Just like the skeleton for your body, the cytoskeleton (“cyto” meaning cell) does the same for all cells in your body. Unlike our body’s skeleton, the cytoskeleton plays an important role in transporting cargo (which can be protein, cellular vesicles and RNA) from one part of the cell to another. This transport process is known as axonal transport and is known to be disturbed in ALS patients. The cytoskeleton works by providing the “rails”, similar to railroad tracks, in which the cargo can be transported. Also comparable to railroad tracks, defects in the cytoskeleton (or railroad tracks) will block the transport of this cargo. This is especially important in motor neurons, where the axons can be as long as three feet.
Cytoskeletal alterations are a common pathological feature in ALS patients. The identification of cytoskeletal genes that are associated with ALS establish that cytoskeletal defects are a major pathway contributing to ALS pathogenesis. A major focus of our laboratory is to further dissect how such alterations lead to disease pathogenesis. Towards this goal, we are working with model organisms, which have proven to be a tremendous resource for the study of human diseases. We focused on the development of murine models of ALS based on our identification of mutations in PFN1 and TUBA4A. In collaboration with Dr. Zuoshang Xu at UMass, we completed the development of a transgenic mouse that expresses mutant PFN1. Interestingly, this model demonstrates several of the characteristics of ALS, including late onset progressive paralysis, decreased weight, decreased grip strength and motor neuron loss. Additionally, in collaboration with Jackson Laboratory, we have developed mice that harbor point mutations in TUBA4A using CRISPR technology. Undoubtedly, these mouse models have opened up several new avenues of research to further understand the pathogenesis of ALS with a focus on cytoskeletal defects. These include the study of disease development and progression, changes in gene expression over time and examining how cytoskeletal defects lead to alterations in other cellular processes. As such, we anticipate that the study of these models will be a major focus of our laboratory to study cytoskeletal defects in ALS for the foreseeable future.