Fellowship Goals and Objectives
With supervision, fellows will serve as consultants as part of our interdisciplinary team of physicians, nurse practitioners, social workers, nurses and music therapists with a biopsychosocial-spiritual approach to patient and family care.
As the year progresses, fellows take a leadership role on the team by facilitating daily rounds. Over time, fellows will be expected to teach on palliative care topics at weekly team meetings, resident conferences, and at the bedside with students, residents and visiting fellows from oncology to critical care and geriatrics, among others.

First week with our new 2024-25 fellows: (left to right) Sara Lyon RN, Philip Hewes MD (fellow),
Vandana Nagpal MD, Marie King MD (fellow) and Pamela Lane NP
- Fellows will apply broad medical knowledge of pathophysiology and management of common serious illnesses (cancer, heart failure, chronic obstructive lung disease, chronic kidney disease, liver disease, dementia and geriatric frailty, etc.) to controlling complex pain and symptoms with pharmacologic and non-pharmacologic treatments.
- Fellows will facilitate patient-family meetings to explore understanding of illness, prognosis, values, and goals to develop goal-concordant treatment plans across settings of care.
- Fellows will recognize and address emotional, psychosocial, existential and spiritual suffering as well as financial and practical needs in collaboration with the interdisciplinary team.
- Fellows will demonstrate consultant etiquette by working collaboratively with the referring doctor or team, other consultants, the patient, the family and other palliative care team members and assist with safe and effective transitions in care.
- Fellows will develop skills in conflict resolution and apply a rigorous ethical framework to negotiating complex medical decisions, especially at end of life.
- Fellows will recognize and explore the cultural, spiritual and socioeconomic factors impacting their patients’ care, including trauma from systemic racism and social and health inequities.
- Fellows will develop self-care and resiliency skills in caring for seriously ill or dying patients with support from the interdisciplinary team.
- Fellows will understand and articulate the key metrics for measuring quality of palliative care and program growth, as well as advocate for palliative care with effective messaging to clinical colleagues, patients, families and community members.
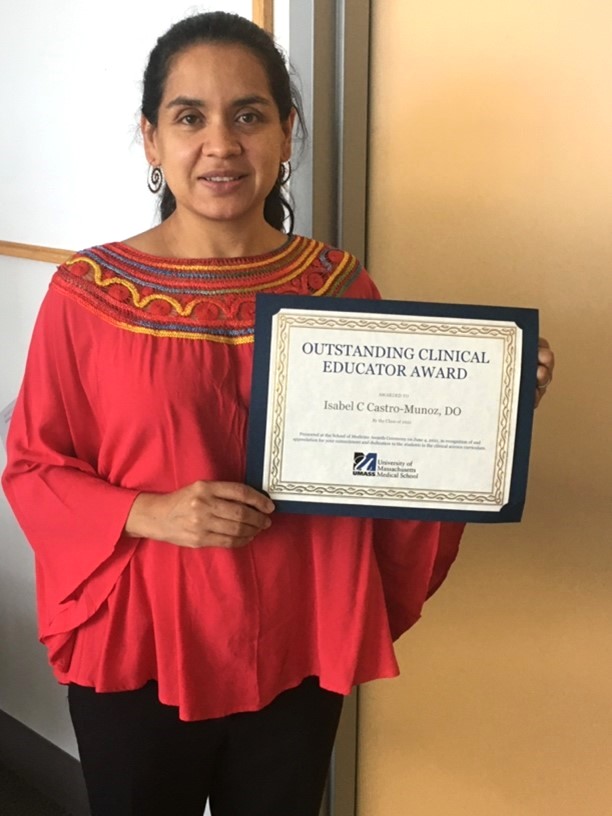
Isabel Castro, DO, with her teaching award from medical students.