Antibody blockade of IL-15
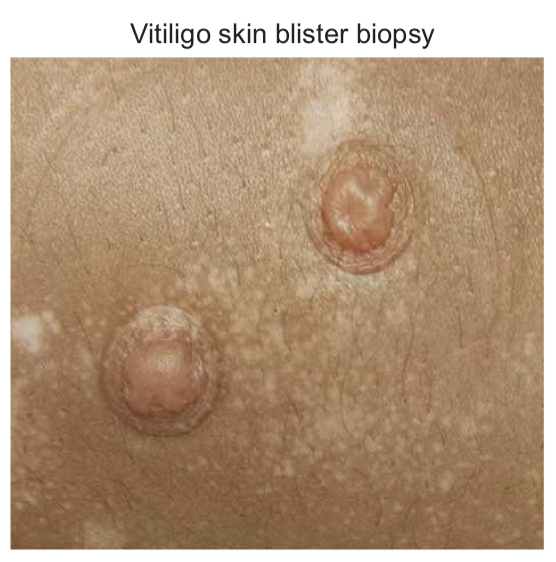 Vitiligo is an autoimmune disease of the skin that causes disfiguring white spots, which can appear anywhere on the body. Existing treatments, which are used “off-label” because they have not been FDA-approved to treat vitiligo, can be effective for patients. These treatments reverse the disease by stimulating brown spots to appear around hair follicles within the affected skin, which then increase in number and size until the white spot has disappeared, replaced with normal skin color. However, in most cases when treatments are stopped the disease relapses, meaning that the white spots reappear at the same location they were prior to treatment. Thus, we hypothesized that autoimmune memory forms within the skin when the spots appear, so that the spots “know” where to return when treatments are stopped.
Vitiligo is an autoimmune disease of the skin that causes disfiguring white spots, which can appear anywhere on the body. Existing treatments, which are used “off-label” because they have not been FDA-approved to treat vitiligo, can be effective for patients. These treatments reverse the disease by stimulating brown spots to appear around hair follicles within the affected skin, which then increase in number and size until the white spot has disappeared, replaced with normal skin color. However, in most cases when treatments are stopped the disease relapses, meaning that the white spots reappear at the same location they were prior to treatment. Thus, we hypothesized that autoimmune memory forms within the skin when the spots appear, so that the spots “know” where to return when treatments are stopped.
We and three other laboratories searched for autoimmune cells that might be the source of this remaining disease memory in the skin. We looked in the skin of vitiligo patients as well as the skin of mice that get vitiligo, and discovered that “resident memory T cells”, or Trm, form within affected skin immediately when the white spots appear and remain at that location for a long period of time afterward. Similar cells form in the skin after a viral infection and are responsible for protecting the skin from reinfection in case the virus comes back again. We then hypothesized that if these cells could be removed from the skin, the disease would get better and this improvement would be long-lasting, since the autoimmune memory would be removed with them.
Next, we looked for an “Achilles’ heel” of these cells that we could target therapeutically. We determined that the vitiligo-causing Trm cells required a cytokine protein called IL-15 for their survival and found that blocking the signaling of this cytokine in with an antibody treatment removed the Trm cells from the mouse skin and resulted in significant improvement in their skin. Importantly, even short-term treatment of the mice resulted in long-term, or durable, improvement, suggesting that this treatment strategy, unlike existing treatments, might provide lasting benefit for vitiligo patients. It also seemed to target only the autoreactive cells, not the normal ones, because the autoreactive cells were more dependent on IL-15 than the others. Studies in human vitiligo patients seemed to support this as well, suggesting that this therapy might be safer for the immune system than first thought.
