Since the outbreak of the coronavirus pandemic in late 2019, the evolution of COVID-19 management has changed for both individuals and the greater population. Today, vaccines and antiviral treatments like Remdesivir and Paxlovid are available, and herd immunity has been achieved through vaccination and natural infection.
Still, COVID and long COVID remain a concern, especially for people with comorbidities. The Massachusetts Department of Public Health recommends oral antivirals as a first-line treatment for people with COVID who are at higher risk of severe disease, with IV antivirals as an alternative.
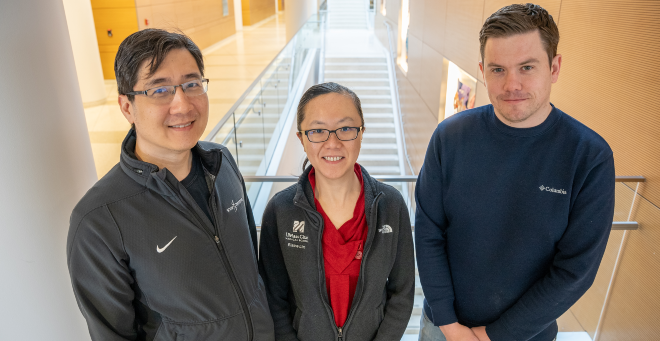
We spoke with infectious diseases and immunology expert Sandeep S. Jubbal, MD, assistant professor of medicine, on the state of COVID today, vaccines, the role of at-home tests in diagnosis, and his recommendations for people diagnosed with COVID-19 or long COVID.
Q: It’s been nearly five years since the start of the coronavirus pandemic. Where are we now and what are we still facing? Are there any underlying issues that we still have to worry about? And what about the possibility of another outbreak? Are we passed that?
Dr. Jubbal: Things have changed, obviously. Initially, when it all started, we didn’t have any treatment options. Now we’ve got great vaccines. We’ve got plenty of treatment options. We have reached a level of herd immunity, both via vaccine and natural infection. From what I’ve seen, patients have stopped checking or testing themselves for COVID-19 unless it’s required from their employer. Over the past four or five years, there have been a couple of trends. There’s the summer trend and the winter trend, which happens soon after Thanksgiving.
The number of patients has gone down compared to what we were dealing with three or four years ago, and I think it’s a mix of herd immunity, mild infections and mostly because people aren’t testing.
Q: Is long COVID something that people should be more worried about now than in previous years? And are the symptoms generally the same as they were years a couple of years ago?
Jubbal: With long COVID, there’s a lot of research that is ongoing, and we are getting preliminary results. Anybody who has any comorbidity or has any high risk for disease progression, I do recommend getting treated because we want to get rid of this virus from the system as soon as we can, just because of the risk of long COVID. I know the symptoms may be mild. The patients might not have severe symptoms needing hospitalization or an emergency visit, but still, there’s always this risk of this unknown, long COVID phenomena, which makes me a little concerned.
Q: Beyond older adults, people with diabetes or heart conditions, are there any additional groups of people that have been identified in the past few years who might be more susceptible to COVID than others?
Jubbal: From my experience, I’ve identified anybody who has a high BMI, has a higher risk of disease progression, are transplant patients, are on heavy dose immunosuppressive agents, or are on active chemotherapy.
Q: What do you recommend for people who test positive for COVID-19?
Jubbal: A mix of monoclonal antibodies, like Remdesivir, which is the current approved antiviral treatment, and the oral antiviral pill, Paxlovid. I have been very liberal in providing these treatments just for the sake of getting this virus out.
I strongly believe that everybody should be treated, just because these treatments are very safe and there are no side effects associated with these treatments.
The number one guidance from the National Institutes of Health and the Commonwealth of Massachusetts says everybody should be assessed for oral antivirals. But if there’s some form of drug interaction or side effect, then we usually call them in for IV antiviral, which is Remdesivir. The problem with Remdesivir is that it has to be given for three successive days, and right now we are sending those patients to the emergency room.
Q: What steps should a person take after testing positive?
Jubbal: Anyone who tests positive, whether they have comorbid conditions or not, should reach out to their primary care physician. From what I’ve seen, primary care physicians have been very good in terms of prescribing oral antiviral agents.
Q: What about at-home tests? Are they still considered reliable?
Jubbal: There have been great at-home tests. Along with vaccines, they have been a game changer. Whatever success we have achieved in this pandemic, they have a huge role to play.
Q: A new vaccine rolled out in late August. When it comes to this new vaccine, what are your recommendations for people with comorbidities or vaccine hesitancy?
Jubbal: I strongly recommend vaccines. People are likely wondering why we’re getting so many vaccines. The answer is because the immunity is very short lived, maybe three or four months. That’s why for somebody who is severely immunosuppressed, because of the medications they are on or from their disease, we strongly recommend getting the booster. This vaccine not only provides a protection against the original COVID strain, but also the new variants, which are predominant currently in the United States.
The rate of hospitalization has gone down considerably for vaccinated patients who have been on chemotherapy or who are on immunosuppressive medications. Mortality rates have gone down.
Vaccines, hands down, are effective. They might not prevent the spread of infection as much as they can definitely prevent hospitalization and mortality.
Dr. Jubbal joined UMass Chan in 2015. He is an assistant professor of medicine in the Division of Infectious Diseases and Immunology. He serves as the medical director of the COVID Treatment Center at UMass Memorial Medical Center and is the secretary for the Commonwealth of Massachusetts’ Board of Registration in Medicine.