Researcher Spotlight: Sambra Redick, PhD - Creating Stem Cell-Derived Pancreatic Islets
Date Posted: lunes, marzo 27, 2023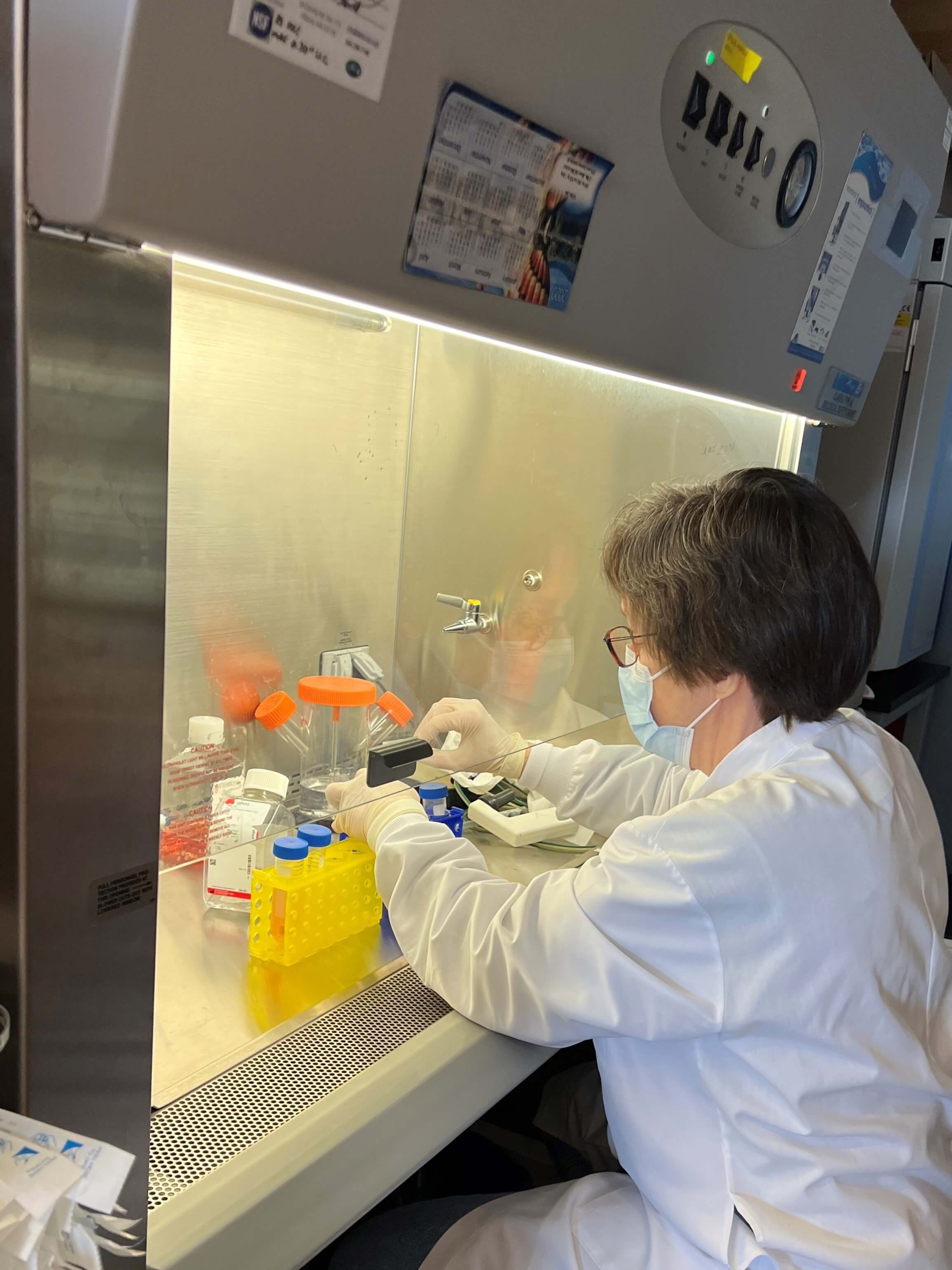
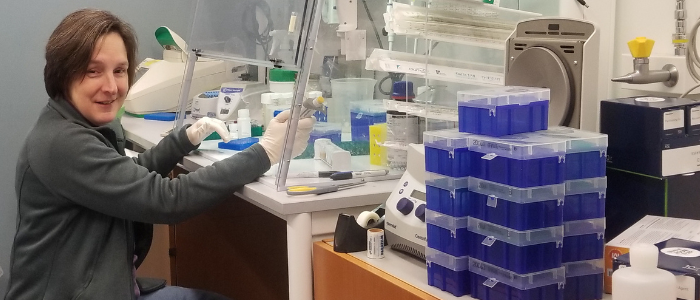
Sambra Redick, PhD is a senior research scientist in the laboratory of Dr. David Harlan. Since arriving at the UMass Chan Diabetes Center of Excellence (DCOE) in 2015, she helped put to rest a decades old debate about beta cells. In collaboration with engineers at Worcester Polytechnic Institute (WPI), she developed a novel tool to improve the removal of individual islets from human pancreas slices to better investigate them. Dr. Redick is focused on functional and transcriptional profiling of pancreatic islets from both diabetic and non-diabetic donors. She has developed techniques to remove and study single islets from slices of human pancreas that we receive as members of the Network for Pancreatic Organ Donors with Diabetes (nPOD), and uses methods that allow her to obtain transcriptional profiles of single cells from within those islets.
In 2023 Dr. Redick led the effort to develop a Stem Cell Islet Core at the UMass Chan DCOE to grow stem cell-derived islets to be used for various collaborative research projects. The Harlan lab is focused on insulin producing beta cells and what they may be doing to attract the attention of the immune system to create the autoimmune attack of type 1 diabetes (T1D). They work closely with the laboratory of Sally Kent, PhD, who studies T cells to investigate those immune cell’s role in the process.
When the DCOE receives pancreas samples for study, each lab investigates their cell type of interest. The laboratories of Michael Brehm, PhD and Dale Greiner, PhD utilize novel "humanized" mouse models to observe human cells and tissue in vivo. The goal is to understand T1D pathogenesis in order to develop new therapies for personalized medicine.
These scientists and ten others from the UMass Chan DCOE, Harvard Medical School, Boston Children's Hospital and The Jackson Laboratory comprise a New England collaboration, led by Dr. Harlan, who are working to genetically modify stem cell-derived islets so that they become undetected by the immune system. Those engineered cells are tested in “humanized” mice to determine their functionality in vivo.
Transplanting stem cell-derived islets into a person with type 1 diabetes, without requiring toxic immunosuppressive therapy, would be a life-changing curative therapy. That is the core focus of the Breakthrough T1D (formerly JDRF) Center of Excellence in New England.
Type 1 Diabetes Researcher Spotlight: Sambra Redick, PhD
Sam’s interest in cell biology stems from a 4th grade science project she did on the topic of DNA replication. She grew up in South Carolina and became the first person in her family to finish college.
After serving in Japan during World War II, her father became a self-educated electronics and pneumatics mechanic at a paper mill. Sam’s mother began working in a dress factory while still in high school and worked her way up to a position in motion economy, determining the most efficient way to cut and assemble dresses.
“My folks always told me I was going to college, and I decided in junior high that I wanted to attend college, but not just to get one degree, I wanted to get them all,” she said with a smile.
Sam studied genetics at University of Georgia, then earned both her master’s degree and PhD in molecular biology at Princeton University where she had planned to study virology. “By that time, I thought transcription would be very important and control a lot of biology.”
Students were required to do three rotations to experience a variety of labs before committing. Sam’s final rotation was in a laboratory that studied the extracellular matrix, which is secreted by cells and regulates processes by controlling cell communication. “I was hooked,” she said. “Much of the extracellular communication that passes through a cell involves the matrix in some way.”
Her first postdoctoral fellowship was at the University of North Carolina working in a lab that used mouse embryonic stem cells to study blood vessel development.
 Sam realized early on that she didn’t aspire to run her own lab, but rather enjoys performing research at the bench. “I like working with my hands doing the physical experiments, and I love troubleshooting,” she said.
Sam realized early on that she didn’t aspire to run her own lab, but rather enjoys performing research at the bench. “I like working with my hands doing the physical experiments, and I love troubleshooting,” she said.
Her second postdoc position was at Duke University in a lab that was working on two completely different projects. “At that point I didn’t necessarily care what the project was,” she said. “I just wanted to investigate interesting questions and use cool tools!” She got some papers published about cell adhesion and anti-adhesion, and then transitioned to the bacterial cell division side of the lab.
Joining UMass Chan Medical School and the Diabetes Center of Excellence
She first arrived at UMass Chan Medical School in 2003 working in the laboratory of Dr. Stephen Doxsey. They studied cell division with a focus on the centrosome and mitotic spindle poles. After 12 years in the Doxsey Lab, funding ran dry and Sam’s network on campus led to a position in the Harlan Lab in the UMass DCOE.
At that time, they obtained donated pancreatic islets from deceased diabetic and non-diabetic donors and separated them into single cells. Those cells were stained and sorted into cell groups by hormones (insulin, glucagon, etc.). Sam performed RNA-sequencing to examine the transcriptome of those cells to determine their messenger RNA molecules. The Harlan Lab was looking for differences between beta cells from the islets of people who had T1D and those who were non-diabetic. They compared cells from people who passed away during various phases of the disease process to investigate changes in gene expression and compared them to cells from people without diabetes. The goal was to understand if beta cells do something to attract the attention of immune cells, thus causing the autoimmune attack, or if perhaps beta cells are simply “innocent bystanders.”
They soon determined that sorting cell groups by insulin could be missing important information since beta cells from people with T1D didn’t produce much insulin. Dr. Redick started working on new techniques to interrogate single cells without regard to hormone expression. Today they capture the cells from islets using a molecular biology process that captures single cells and labels the individual gene expression of each. This process continues to produce gigabytes of data to be analyzed by our bioinformatician to identify cell types by their gene expression hallmarks and examine how the individual gene expression profiles vary.
Resolving a 30-year debate by locating beta cells in people with T1D that express important immune pathway gene products
By far the greatest genetic risk for T1D is driven by the expression of immune genes called “human leukocyte antigen class II” (HLA Class II) and yet human beta cells were thought by many, not capable of expressing HLA Class II and other important genes supporting HLA Class II function. Collaborative research in the Harlan Lab definitively showed that beta cells from individuals with T1D express these important gene products. Since they are immune system genes, it raised the question of whether this immune function is an important part of what T cells are seeing to trigger the autoimmune attack on beta cells.
Creating a tool to procure single islets
The Harlan lab feels that since diabetes is a patchy disease with varying effects on islets that have widely varied sizes and cellular composition, studying single islets will be beneficial if we can investigate them individually. Dr. Redick has developed techniques to separate single islets including a halo of T cells around the edge of the islet, allowing them to study the importance of that ring of immune cells. They’ve developed a novel tool to punch and recover individual islets from living pancreas slices for more in-depth investigation.
About Sam
Sam and her husband share their home with two cats. She enjoys growing a garden at home, especially vegetables that aren’t available locally. “I’m a southerner, so we have a big okra patch, purple top turnips with the greens on,” she said. “All the cliches of southern food.” She enjoys cooking and compared it to lab work, because you follow a protocol, except “the experiment almost never fails so badly that you can’t have dinner,” she joked.
Sam’s favorite part of living in New England are the four seasons. She enjoys fall foliage, winter sports like cross country skiing, and spring & summer activities such as hiking, kayaking, cycling and other outdoor activities.
Favorites
TV Shows: M.A.S.H., Star Trek Next Generation, Big Bang Theory
Movies: The Princess Pride, Harold and Maude
Restaurants: Eller’s for breakfast, Fatima’s Café, Nancy Chang’s, BT’s Smokehouse
Hobbies: She is a steam team train enthusiast
Related Articles
Modeling Type 1 Diabetes Using Human Stem Cells in the Brehm and Greiner Labs
Researcher Spotlight: Carey Zammitti - Humanized Models of Type 1 Diabetes
Researcher Spotlight: Bioinformatician Mason Tarpley
