Advanced Mental Health Care in Primary Care
*Psychologists, Social Workers, and Counselors please refer to the Certificate Course in Primary Care Behavioral Health
This course is designed for
Physicians, Nurse Practitioners, and Physician Assistants
Why do you want to take this course?
Most mental health care in the United States occurs in primary care.1 Clinicians who specialize in primary care are passionate about whole-person health and want to care for the physical and mental health needs of their patients, which is aligned with what patients are seeking from their PCPs. Graduate medical training, residency, and fellowship training provide a foundation for addressing a patient's mental health needs, but many primary care clinicians feel their training did not fully prepare them to treat the complex mental health needs of their patients.2,3
Primary care clinicians also face resource scarcities and structural barriers that hinder their efforts to address mental health conditions. There never seems to be enough time, staffing, and reimbursement, in addition to the training limitations faced by most clinicians. Efforts to improve access to competent and compassionate mental health care must be multipronged, with primary care playing a pivotal role. Many factors are outside clinicians’ control, but gaining the skills necessary to screen for, diagnose, treat, and monitor mental health conditions can empower primary care clinicians to provide better care to more of their patients while promoting greater job satisfaction on a daily basis.
Over the past decade, CIPC faculty have experienced firsthand the increasing need to enhance mental health training and education available to medical and nursing clinicians in primary care. This course responds to that need in a form that is accessible and targeted at exactly the information PCPs want and need to know.
The Certificate in Advanced Mental Health Care in Primary Care course was developed for physicians, physician assistants, and nurse practitioners who work in primary care and want to increase their confidence, knowledge, skill, and capacity to treat mental health conditions. Created by an interdisciplinary group of experts, our faculty are practicing clinicians and educators in primary care with extensive experience at the complex intersections of psychiatry, psychology, structural and social determinants of health, and primary health care.
The course addresses the real-life, complex patient presentations we see in primary care everyday. Thematically integrated throughout is content that acknowledges and responds to the daily challenges of providing care to populations facing structural health inequities with emphasis on the critical role of chronic stress exposure, trauma, and adversity in the development of mental health conditions. We also center patient stories and lived experiences.
Psychopharmacology is a major emphasis of the course, with content dedicated to providing clinicians with fundamental knowledge about all major psychotropic medication classes and detailed information on how to use individual medications based on different patient factors, co-occurring conditions, and presenting symptoms. You’ll learn how to select the right medication, how to dose it, and how to safely monitor its effects. Learners will also receive comprehensive guides to diagnostic assessment of different conditions, patient-centered communication and engagement, and counseling skills that medical clinicians can utilize in their daily practice.
You will find the course is flexible, engaging, and supportive through a combination of self-paced online content and live learning sessions where learners can interact with faculty, engage in discussion, and ask questions. The course mirrors the clinical work we do everyday and can be summed up by the following:
Person-centered, evidence-informed mental health care, anchored in compassion and humility
Who is this course designed for?
-
Physicians (MD, DO) and Advanced Practice Providers (Physician Assistants, Nurse Practitioners) working in Primary Care Settings
-
Residency and fellowship programs looking to offer a more advanced mental health in primary care curriculum to learners committed to expanding their knowledge and skillset.
-
Nurse Practitioner, Physician Assistant, & Medical Students committed to pursuing careers in primary care.
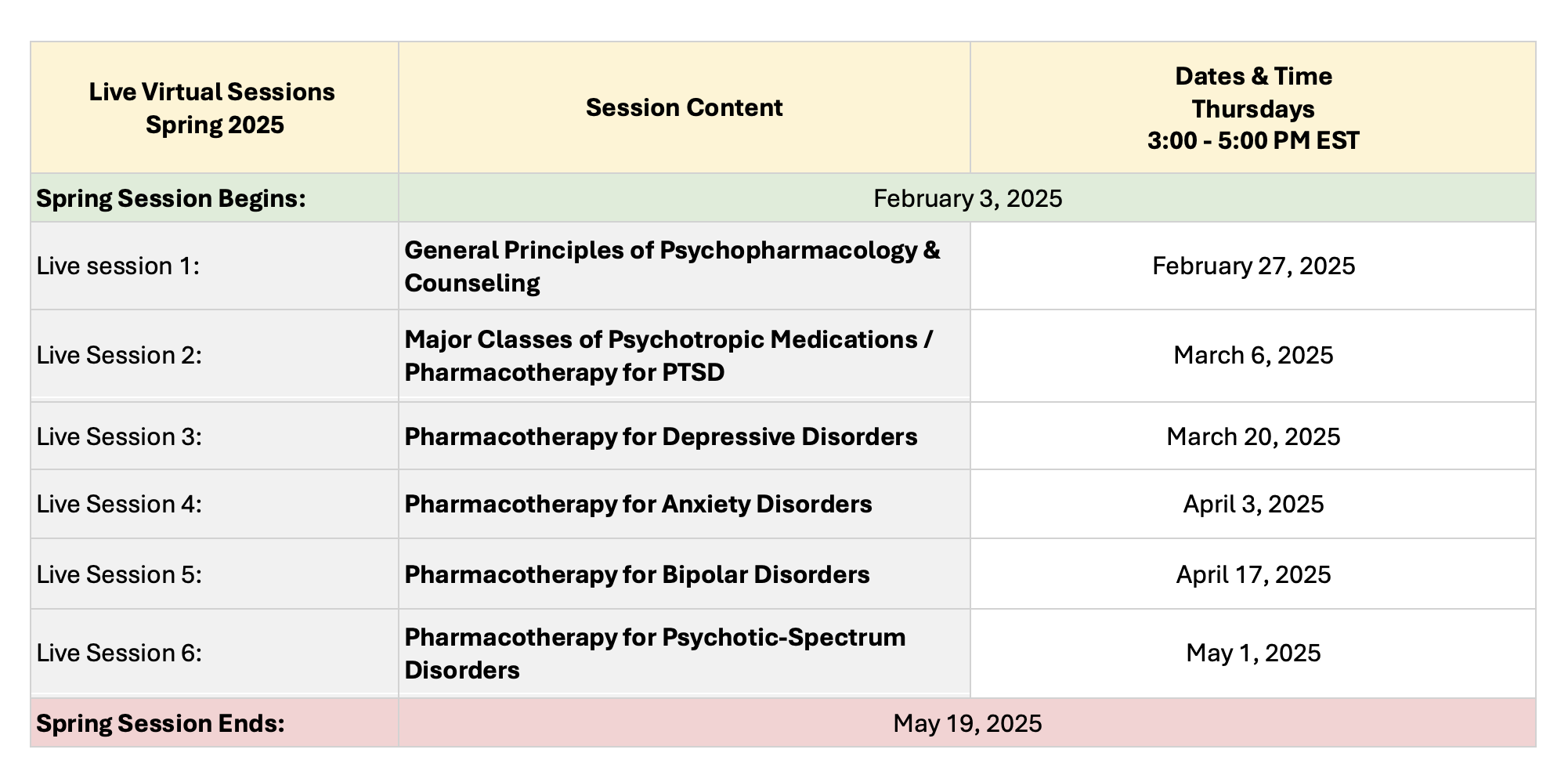
When does this course occur?
- This course will run two sessions per year: Fall & Spring
- The entire course is delivered online, no travel to Massachusetts is necessary
- Spring 2025 Session:
- Starts: February 3, 2025
- Ends: May 19, 2025
- Enroll by: February 15, 2025
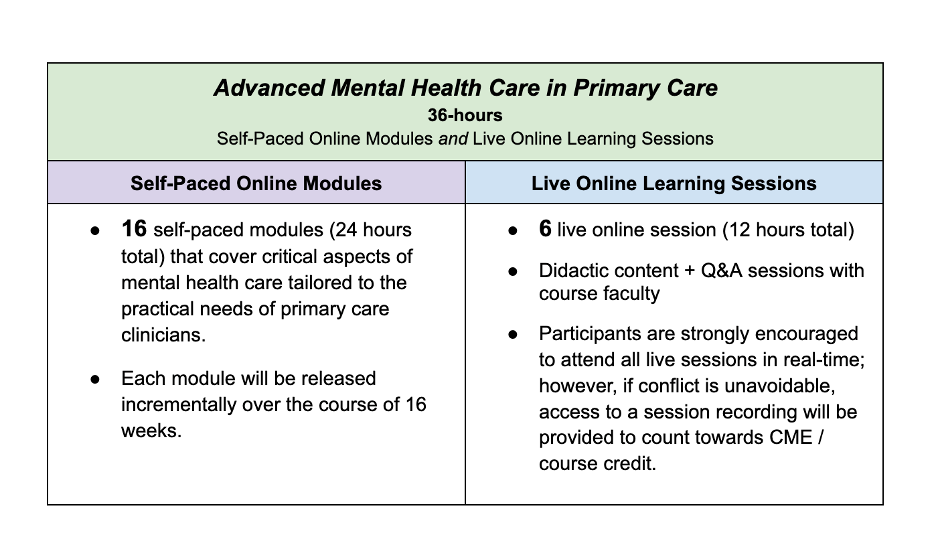
Overview of Course Format:
Cost:
- $1,800 per person
- Group rate 10+ = $1,600 per person
-
Discounted rates are available to UMass Affiliated Faculty & Trainees. Reach out to a learning specialist to inquire about a discount
Review our refund policy here
Continuing Medical Education Credits:
 |
Provided by: American Academy of Family Physicians This session, Advanced Mental Health Care in Primary Care, AAFP Prescribed credit is accepted by the American Medical Association as equivalent to AMA PRA Category 1 credit(s)™ toward the AMA Physician's Recognition Award. When applying for the AMA PRA, Prescribed credit earned must be reported as Prescribed, not as Category 1. |
Course Faculty:
- Jordan Howard-Young, MD, MA-ID, DAAETS (he/they)
- Amber Cahill, PsyD (she/her)
- Marie Hobart, MD (she/her)
- Learn more
Enroll by February 15, 2025
References:
- Jetty A, Petterson S, Westfall JM, Jabbarpour Y. Assessing Primary Care Contributions to Behavioral Health: A Cross-sectional Study Using Medical Expenditure Panel Survey. J Prim Care Community Health. 2021;12:21501327211023871. doi:10.1177/21501327211023871
- Wakida EK, Talib ZM, Akena D, et al. Barriers and facilitators to the integration of mental health services into primary health care: a systematic review. Syst Rev. 2018;7(1):211. Published 2018 Nov 28. doi:10.1186/s13643-018-0882-7
- Poghosyan L, Norful AA, Ghaffari A, George M, Chhabra S, Olfson M. Mental health delivery in primary care: The perspectives of primary care providers. Arch Psychiatr Nurs. 2019;33(5):63-67. doi:10.1016/j.apnu.2019.08.001