Posted On: March 08, 2021

Dr. Ethan Eisdorfer, a behavioral health provider at our Barre Family Health Center, analyzes a recent JAMA article about using non-specialist care providers to deliver brief mental health interventions to pregnant and post-partum women.
The most common types of non-specialists in these studies were midwives and nurses, but also included peers or community members, health visitors, and even family physicians. In many of the studies included in the analysis, professional mental health specialists served in a training or supervisory role without providing any direct care.
What would task-shifting like this throughout primary care practices look like? How might it change the efficiency and efficacy of current healthcare? Click on the title above to learn more.
Posted On: June 15, 2020
Learning to Fly: a journey into teaching and mentoring in IBH

In the midst of a world-wide pandemic, behavioral health needs have grown to epidemic proportions among many who have no history of mental illness, as well as those who have long experienced mental illness. In an analogy that many have used, it often feels like learning to fly while already in the air. From this perspective, I feel compelled, as a health psychologist trained in integrated care, to consider how mental health clinicians may find innovative ways to use their skills in assisting systems of care that need our guidance most.
Posted On: September 15, 2019

Late this spring the CIPC faculty read with interest a special issue of Journal of Clinical Psychology in Medicals Settings on “The Primary Care Behavioral Health Model of Integration”. One particular article caught the attention of CIPC Director, Daniel Mullin. The author, Adrienne A. Williams, PhD discussed in “The Next Step in Integrated Care: Universal Primary Mental Health Providers” the binary view of mental health, either a patient is mentally healthy or is mentally ill. The author cites examples of how this view reinforces stigma associated with seeking mental health services, even within current integrated care models.
Williams suggests as a solution, a primary mental health provider, “In contrast to the binary view, where some people are seen as needing an MHP and others do not, this model would be similar to the primary care model of health and would involve development of primary mental health providers (PMHPs). These PMHPs would be to mental health care what primary care physicians (PCPs) are to physical health care.”
Read More >
Posted On: April 09, 2019
Posted On: April 04, 2019
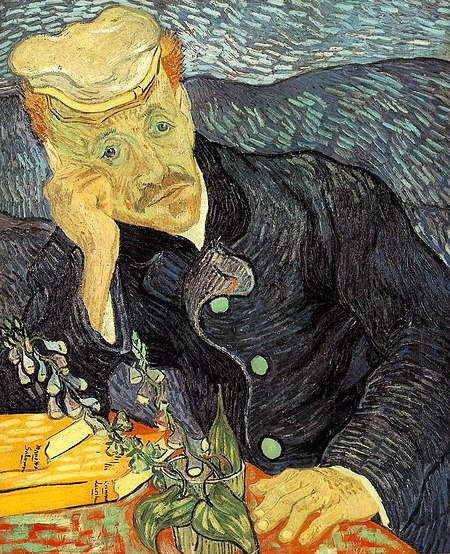
 Our founding director, Dr. Alexander Blount, guest blogs about his new book, "Patient-Centered Primary Care: Getting From Good to Great".
Our founding director, Dr. Alexander Blount, guest blogs about his new book, "Patient-Centered Primary Care: Getting From Good to Great".
Sandy's 1998 volume "Integrated Primary Care: The Future of Medical and Mental Health Collaboration" is one of the foundational texts of the movement to acknowledge the importance of mental health to our physical well-being and to integrate behavioral health care into primary care. Click on the post title to read his blog post explaining how the new volume is the next chapter for IBH.
Posted On: March 27, 2018
Recently, one of our family doctors posted a link to an article in the New England Journal of Medicine about physician burnout, a recently hot topic purporting epidemic levels of physician burnout with not only personal impact but also patient care implications. A nerve was touched.
Posted On: January 18, 2018

One of our recent fellows, Joan Fleishman, PsyD, is the Behavioral Health Clinical and Research Director in the Department of Family Medicine at Oregon Health & Science University (OHSU). She recently co-authored a paper in the Annals of Family Medicine. “Interdisciplinary Management of Opioid Use Disorder in Primary Care” describes a Medication Assisted Treatment (MAT) program in the Pacific Northwest.
Posted On: December 28, 2017
 The team-based skills needed for effective behavioral health integration into Primary Care require specific competencies. Read how our founding director, Dr. Alexander Blount is helping to shape what we mean by "competencies".
The team-based skills needed for effective behavioral health integration into Primary Care require specific competencies. Read how our founding director, Dr. Alexander Blount is helping to shape what we mean by "competencies".