Projects

Signature Project
Jaspr: Testing and Implementing a Tablet-based Intervention to Support Patients with Suicidal Thoughts or Attempts in Emergency Departments
Lead: Edwin Boudreaux; Collaborators: Martin Reznek, Chengwu Yang, Ben Gerber
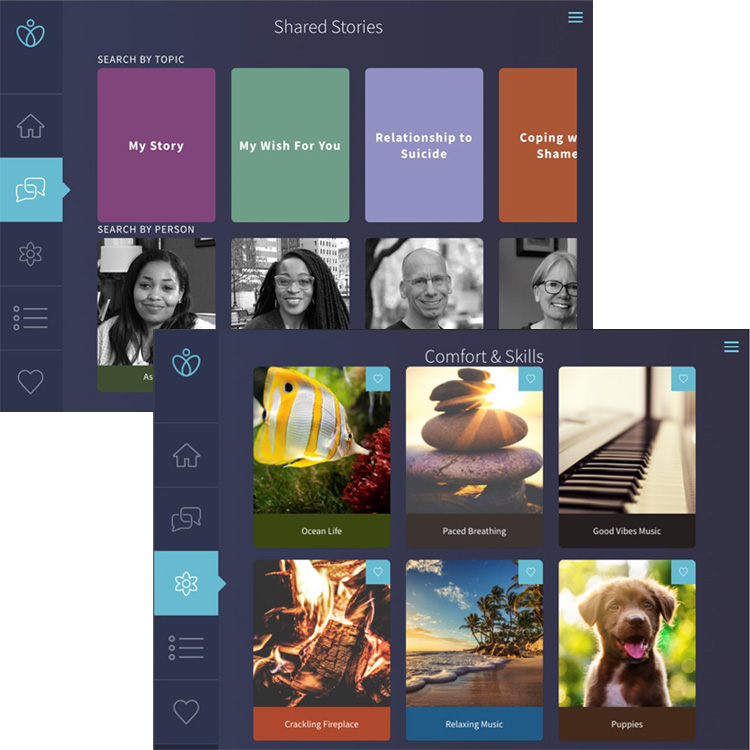
The Jaspr study will evaluate Jaspr Health's patient-facing tablet-based application during suicide-related emergency department visits. The app guides patients in completing the Suicide Status Interview, which comprise of an evidence-based Collaborative Assessment & Management of Suicidality (CAMS) certified suicide prevention tools including a suicide risk assessment, Stanley Brown- inspired safety planning, and lethal means safety counseling. It also offers access to a menu of "Comfort and Skills" modules that teaches patients behavioral skills to effectively manage imminent distress, while shared stories offer a library of professionally produced, racially and culturally diverse, inspirational videos of people with suicide-centered lived experience.

Subjects who interact with Jaspr are encouraged to access their safety plan, comfort and coping skills exercises, and the video library via Jaspr at Home (JAH) mobile application. A summary of the self-administered risk assessment is shared with the clinical team directly through the patient electronic medical record to help guide the treatment plan. The Jaspr app saves clinician time in administering the risk assessment and provides patients with an evidence-based suicide intervention while they await clinical services.
Part A of the study will be an individual, patient-level randomized controlled trial at UMass Memorial to evaluate the efficacy and mechanism of action of the Jaspr intervention, compared to emergency department treatment as usual. All subjects will complete a baseline assessment prior to random assignment. All subjects will receive follow-up phone calls 6, 12, 24, 36, and 52 weeks after enrollment. These calls will assess suicide related outcomes and healthcare utilization. In addition, the Massachusetts Department of Public Health death registry and each subject's electronic health record will be reviewed for suicide-related mortality and admissions, respectively.
Part B of the study will be a Real-World Study to evaluate the effectiveness and implementation processes in EDs and outcomes. Two health systems affiliated with Ohio State University and the University of Colorado will implement Jaspr as part of routine clinical care. Each health system will implement Jaspr in two diverse EDs: one major academic site and one community site. Each system will collect data on eligible patients across two Phases: (1) a retrospective enhanced treatment as usual phase comprising 12 months of index emergency department visits with a 12-month follow-up window, and (2) an Implementation/Intervention phase comprising 18 months of index emergency department visits with a 12-month follow-up window.
Additional information about the Jaspr signature project is available on NIH RePORTER.
Exploratory Projects
LEMURS
Co-Leads: Katie Dixon-Gordon, Elke Rundensteiner
Leveraging Early Mental Health Uncovering Risk for Suicide (LEMURS) expands a smartphone app that uses passive smartphone data to derive a suicide risk index, and couples it with an iteratively co-designed clinician facing dashboard and processes to streamline suicide risk screening in college campuses.
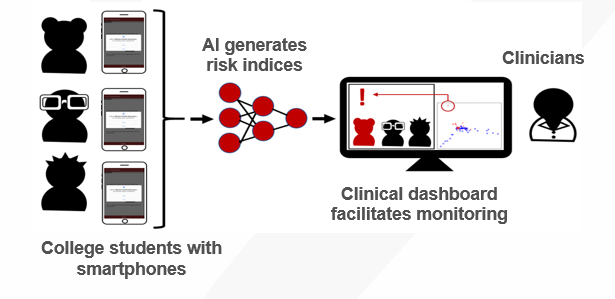
This project, Leveraging Early Mental Health Uncovering Risk for Suicide (LEMURS), extends our work on EMU, which uses passively-obtained data from participants’ smartphones to screen for distress and suicide ideation and extends this to LEMURS which will activate risk alerts in health provider-facing dashboards, and applies implementation science principles for integration and uptake in college health centers. The project has several aims to: (1) understand stakeholder needs and concerns for this technology via interviews with students, clinicians, and staff; (2) co-develop a provider-facing dashboard responsive to student preferences and clinician workflow needs via iterative interviews and prototype evaluations; (3) explore how LEMURS can integrate with suicide risk interventions; and (4) evaluate feasibility/barriers by deploying LEMURS in a college healthcare setting in 40 students (n=20 with high suicide risk) alongside daily surveys evaluating self-reported suicide risk. This project will explore system, clinician, and patient influences on implementation. The goal of this study is to streamline universal suicide risk screening and monitoring of college campuses plagued by a high rate of onset of suicidal thoughts/behaviors. Accelerated translation of LEMURS for suicide risk screening adoption in college health settings has the potential to ease the burden on health systems and reach thousands of at-risk students annually.
Additional information about LEMURS is available on NIH RePORTER.
ADAPT
Co-Leads: Anthony Rothschild, Feifan Liu; Collaborator: Ben Gerber
The Automated, Data-Driven, Adaptable, and Transferable Learning for Suicide Risk Prediction Project (ADAPT), aims to systematically assessing and improving a suicide risk algorithm’s generalizability and adaptability from an original development setting to a new healthcare system.
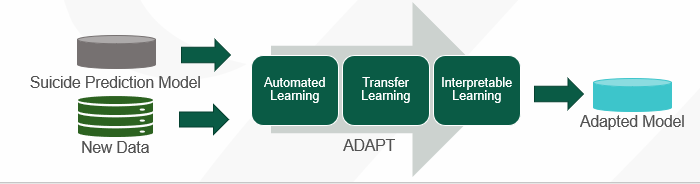 Machine learning algorithms predicting suicide and suicide attempts have demonstrated promising results. However, lack of large-scale external validations, transfer guidance, and automated learning-based adaptation impedes adoption in clinical practice. ADAPT aims to address the translation gap from research to clinical practice by assessing and improving the generalizability and adaptability of the NIMH-funded Mental Health Research Network (MHRN) suicide risk prediction algorithm when transferred to a different healthcare system, by building an innovative adaptation pipeline, ADAPT, for an scalable and automated end-to-end solution to optimally adapt existing suicide risk prediction models to a new healthcare context and in different clinical settings. We will explore strategies to fill potential performance gaps via model adaptation and advanced deep learning methods. The Specific Aims are to (1) assess the generalizability and adaptability of MHRN risk algorithms for suicide risk prediction (2) develop a unified pipeline of Automated, Data-driven, AdaPtable, and Transferable learning (ADAPT) for suicide risk prediction, (3a) to explore an innovative deep learning approach for suicide risk prediction, and (3b) to engage diverse stakeholders to assess ADAPT’s usability, acceptability, and feasibility, as well as potential barriers and facilitators to implementation.
Machine learning algorithms predicting suicide and suicide attempts have demonstrated promising results. However, lack of large-scale external validations, transfer guidance, and automated learning-based adaptation impedes adoption in clinical practice. ADAPT aims to address the translation gap from research to clinical practice by assessing and improving the generalizability and adaptability of the NIMH-funded Mental Health Research Network (MHRN) suicide risk prediction algorithm when transferred to a different healthcare system, by building an innovative adaptation pipeline, ADAPT, for an scalable and automated end-to-end solution to optimally adapt existing suicide risk prediction models to a new healthcare context and in different clinical settings. We will explore strategies to fill potential performance gaps via model adaptation and advanced deep learning methods. The Specific Aims are to (1) assess the generalizability and adaptability of MHRN risk algorithms for suicide risk prediction (2) develop a unified pipeline of Automated, Data-driven, AdaPtable, and Transferable learning (ADAPT) for suicide risk prediction, (3a) to explore an innovative deep learning approach for suicide risk prediction, and (3b) to engage diverse stakeholders to assess ADAPT’s usability, acceptability, and feasibility, as well as potential barriers and facilitators to implementation.
Additional information about ADAPT is available on NIH RePORTER.
CATS-PC
Co-Leads: Rachel Davis-Martin, Bengisu Tulu; Collaborator: Sharon Johnson, Daniel Mullen
Implementing Computerized Adaptive Tests for Mental Health Screening in Primary Care (CATS-PC) applies a person-centered design approach to optimize effective primary care clinical workflow integration of multidimensional computerized adaptive tests (CATS) for identifying and tracking mental health symptoms and suicide risk and guiding intervention delivery.

Through key informant interviews across the country in diverse clinical settings, we will (1) identify effective approaches to implementing computerized adaptive tests (CATS), specifically the CAT-MHTM, for mental health and suicide screening in clinical workflows and understand barriers to implementation. Feedback from these interviews will be used to create workflow designs and results displays for (2) user testing in a simulated clinical environment with standardized patient encounters. The workflow and results display indicated as most acceptable will then be (3) piloted in one integrated primary care for real-world testing. Following this pilot of CAT-MHTM, we will evaluate the feasibility of EHR integrated CAT-MHTM workflows and create a deployment package with implementation tools and considerations for practices that want to deploy CATS to replace existing mental health screeners.
Additional information about CATS-PC is available on NIH RePORTER.
Pilot Projects
The CAPES Pilot Program helps established and emerging CAPES scholars with a small (R03 sized) grant to rapidly advance the science to practice translation, technology translation or technology interventions, and/or implementation science related to suicide prevention in healthcare settings. Only CAPES faculty and Emerging, Established Scholars are eligible to apply for Pilot project funding. Pilot projects work in tandem with our signature and exploratory projects to utilize our existing resources and build upon our knowledge
To apply, CAPES faculty and scholars can email Tony Nunes or refer to the full CAPES R03 RFA sent to your email.
Multisite Validation Study for Suicide Risk Prediction: Integrating the OHDSI Research Network
Lead: Feifan Liu; Collaborators: Ben Gerber, Adrian Zai, Celine Larkin
Promising suicide risk prediction algorithms in research may not be readily translated into clinical practice due to data heterogeneity and healthcare system complexity. Lack of external validation across clinical contexts has delayed their adoption and wider implementation. One of the barriers to multi-site validation is clinical data sharing. Observational Health Data Sciences and Informatics (OHDSI) is an international collaborative whose goal is to create and apply open-source data analytic solutions to a large network of health databases. Based on the Observational Medical Outcomes Partnership (OMOP) common data model, it provides a rigorous and elegant way to validate an algorithm’s generalizability across different institutions without a need for actual data sharing. This pilot study aims to build suicide risk prediction models of the OMOP common data model so that the OHDSI research network can be leveraged for a multi-site validation study.
Optimizing ReachCare for Scalability and Self-Administration
Lead: Rachel Davis-Martin; Collaborator: Celine Larkin; Consultant: Bengisu Tulu
ReachCare is a mobile application that facilitates creation of a safety plan, behavioral outpatient engagement, family support, and values-based living for patients with suicide risk. ReachCare was originally designed for clinician-guided activities that required calls to the patient to create these plans in the app, which hinders wide-spread implementation of the app due to limited clinician resources. This R03 Pilot project aims to update the content of the ReachCare app for self-administration using rule-governed chat bots and will conduct iterative user testing cycles among primary care patients to refine the updated ReachCare app, with additional focus on Hispanic and Latin patients to further improve scalability.
Other Projects by CAPES Faculty
Development and Evaluation of an Avatar Guided Mobile Health for Emerging Adults (EA-Avatar), R00AA029154
Lead: Lourah Kelly
EMERGE: Ecological Momentary Evaluation of Responses to Gain/Loss and Emotions, R01MH128546
Lead: Katherine Dixon-Gordon
Telehealth to Improve Prevention of Suicide (TIPS) in EDs, R01MH124685
Lead: Edwin Boudreaux; CAPES Collaborators: Rachel Davis-Martin, Celine Larkin, Feifan Liu
A System of Safety (SOS): Preventing Suicide through Healthcare Transformation, R01MH112138
Co-Leads: Edwin Boudreaux, Catarina Kiefe
Technology-Assisted Systems Change for Suicide Prevention (TASCS), R34MH123578
Co-Leads: Bengisu Tulu; Celine Larkin; CAPES Collaborators: Soussan Djamasbi, Edwin Boudreaux
